What Health Systems Need to Know About Capacity Optimization
Capacity management in healthcare measures how well health systems can align and allocate their resources—people, facilities, and technology—to meet patient demand. Strong healthcare capacity planning helps reduce wait times, balance provider workloads, and expand access to care. In this article, we explain what capacity in healthcare means, explore common challenges, and highlight digital care orchestration solutions that maximize provider capacity and accelerate growth.

Healthcare capacity management problems often hide in plain sight, and they could be costing your health system more than you think.
What are the signs? Some providers are overbooked, while others have plenty of open slots. Virtual care queues sit empty while in-person Urgent Care and Emergency Department waiting rooms spill over. New specialists struggle to fill schedules while established providers turn patients away.
These capacity management challenges are a major reason why patients across the U.S. healthcare system today wait an average of 31 days to see a provider. But what if you could improve the capacity of your health system by shifting just 5% of low-acuity visits to virtual care … rerouting overflow patients to open slots in real time … and surfacing new providers first in search results to fill out their schedules—fast?
It’s all possible with a capacity optimization platform that orchestrates patient access before bottlenecks occur, enabling health systems to manage demand proactively, match patients with best-fit care, and optimize resource allocation across modalities and sites of care. Let’s take a closer look.
What is organizational capacity in healthcare?
Organizational capacity is your health system’s ability to match patient demand with provider availability. When you get the balance right, you can open up access and achieve sustainable growth.
Doing so, however, is more complex than many health system leaders think. That’s because the meaning of healthcare capacity goes beyond managing inpatient beds. It actually starts where patients enter the system: at the point of search. That’s what makes capacity optimization so effective.
What is capacity optimization?
Different from traditional approaches, capacity optimization focuses on managing healthcare capacity before it becomes a bottleneck. It involves using real-time data to match patients with the right modality, provider, and location at the right time. When done correctly, dynamic capacity management can help your health system care for more patients using its existing resources.
Four key components of a capacity optimization strategy include:
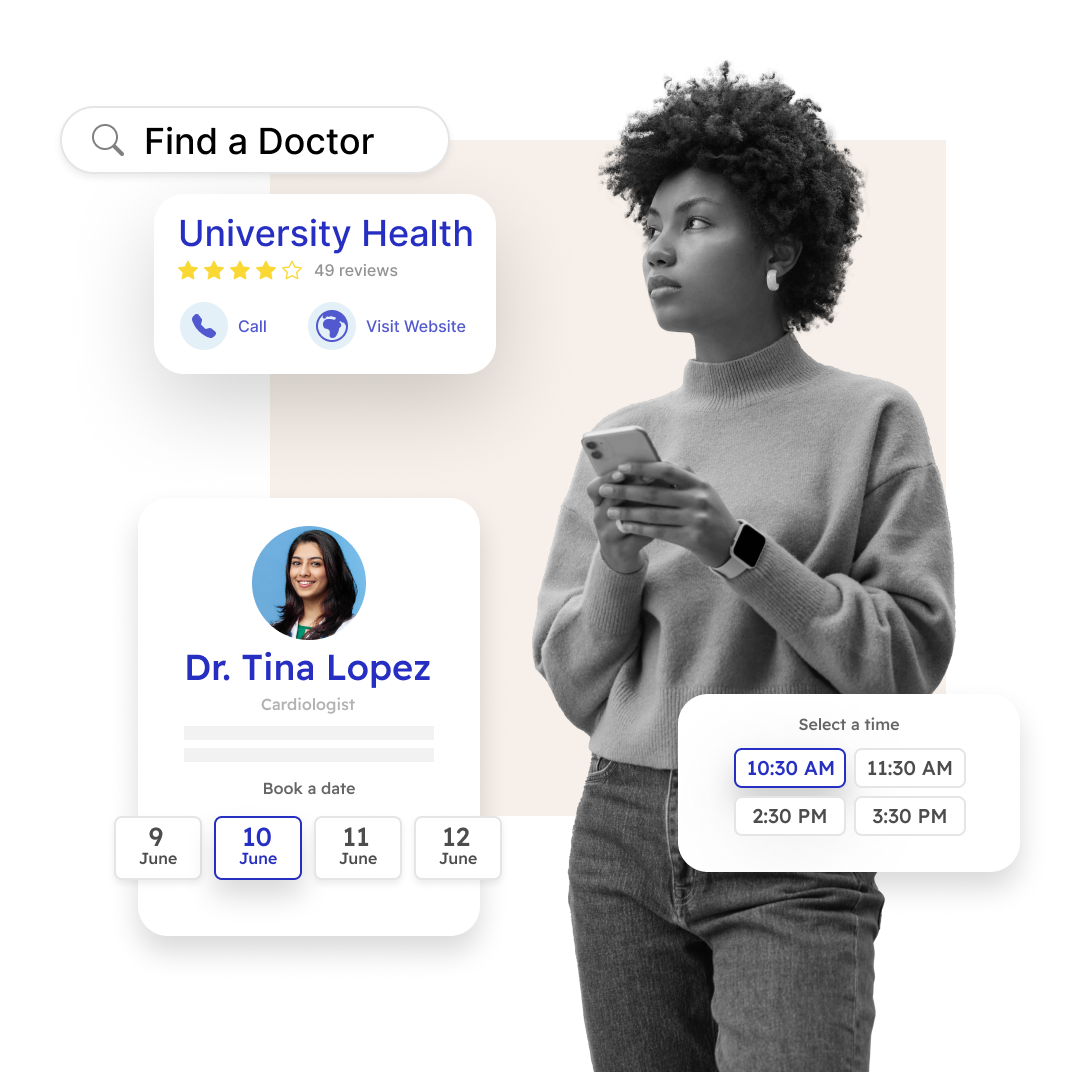
Real-time patient routing based on availability: The right digital tools can match the intent of a patient’s search query with the right providers, sorted by availability and proximity to their home, creating faster patient access with fewer clicks.
Best-fit care options based on acuity level: A patient with symptoms of a sinus infection gets matched with virtual care or a primary care provider instead of an otolaryngologist, ensuring the most appropriate care while preserving specialist resources to handle higher-acuity cases.
Cross-location resource sharing during demand spikes: When one clinic or practice fills up, patients automatically see options at other locations or virtually. No one gets stuck waiting because their preferred location is booked.
Intelligent care setting recommendations: Patients get guided toward virtual visits for appropriate cases, while in-person slots are reserved for conditions that require them, and Urgent Care remains focused on acute needs.
What capacity problems do health systems face?
A few signs that your organization may have hidden healthcare capacity issues include:
Misaligned resources: Not all patients need to see a doctor, but traditional rigid find-a-doctor tools leave it up to the patient to determine which doctor is best. A better approach is using software that matches patients with the provider best suited to manage their case, while also giving physicians the flexibility to see a mix of high- and low-acuity cases.
Geographic imbalances: These happen when one location struggles with scheduling backlogs while another has availability just miles away. Patients assume they have to wait because their preferred clinic is booked, unaware that other providers within your health system have open slots available nearby.
New provider startup headaches: This is an age-old U.S. healthcare capacity problem. Once you hire a new physician, how do you get them booked up quickly? If patients can’t find new doctors easily in search results or scheduling systems, this key resource will go underutilized. Meanwhile, established providers turn away patients that they could refer to their new colleagues.
Seasonal blind spots: A lack of visibility turns predictable patterns into annual capacity management crises. Flu season hits the same time every year, yet many systems react instead of relying on historical data to prepare. Sports physicals spike every August before school starts, creating predictable scheduling crunches that could be anticipated and managed.
Care setting gaps: These occur when Emergency Departments handle low-acuity cases while virtual care queues remain empty. Or when in-person Urgent Care clinics overflow with concerns that could be addressed faster virtually.
The cost of doing nothing about these issues adds up quickly. Each misrouted patient can lead to lost revenue, delayed care, and provider burnout. Capacity optimization addresses all these problems simultaneously.
What are the benefits of capacity optimization?
A recent EY-Parthenon study quantified the potential ROI of capacity optimization efforts. Benefits include:
- Lower costs
- Improved margins
- More free cashflow
- Improved efficiency
These benefits, the report says, make healthcare capacity management an antidote for ongoing financial instability, lagging patient volumes, and increased costs of care at U.S. health systems.
How can health systems gain the capacity to care for more patients?
Leading health systems nationwide are solving their toughest capacity challenges with DexCare’s care orchestration platform. Instead of assessing health system capacity from the inpatient side of the house—after demand hits the system—DexCare takes a proactive approach.
The platform aligns provider workload, care settings, and patient demand from the very first patient interaction, expanding access and accelerating growth by unlocking hidden appointments, reducing bottlenecks, and growing revenue. Here’s how it works:
1. Route patients to the right care setting.
With DexCare, natural language search surfaces the most appropriate care options based on keywords, accounting for the patient’s location, provider availability, and appropriateness of virtual care. By capturing patient intent at their first digital touchpoint, DexCare drives faster access to care.
When patients search for care using everyday language like “sore throat” or “can’t sleep,” the system understands their intent and matches them to the best available option—whether that’s virtual care, Urgent Care, or a primary care appointment.
Capacity management success story
This “front-door” approach to capacity analysis in healthcare is exactly what Piedmont Healthcare achieved when they implemented DexCare. The team created a frictionless booking process with customizable workflows that begins at the point of search and guides patients to the most available and appropriate care options.
The results: A “patient-first” approach to access, reducing time to appointment by 5 days and achieving a 50% conversion rate through cross-sell booking flows.
2. Maximize provider capacity
DexCare shows patients open appointment slots across your entire network and automatically directs them to available providers when their preferred location reaches capacity. The platform displays alternatives across the entire network, surfacing available and hybrid care appointments, so no appointment request hits a dead end.
Capacity management success story
When El Camino Health’s owned clinics reach capacity, patients are seamlessly directed to available slots within their Independent Practice Association (IPA) network. This prevents patients from encountering dead ends while supporting the broader physician community by filling open appointments across all affiliated providers.
The results: Within 90 days of implementing DexCare, El Camino achieved a 130% increase in new patients booked with providers and a 40% increase in total visits scheduled online.
3. Data-driven predictive management
DexCare’s analytics show you where patients are going, which resources are being used, and what demand looks like over time. This data helps you make smarter decisions about where to invest and how much capacity you’ll need. Instead of reacting to problems after they happen, you can spot patterns, predict busy periods, and plan accordingly.
Capacity management success story
SSM Health understood that its patients had to make phone calls just to find out if a provider was available. When customers grew frustrated, they abandoned their search and went to competitors.
The results: Since partnering with DexCare, SSM Health can now use data to serve up options with providers who have availability. This not only helped them balance their physician resources—it also helped them grow new patient acquisition from 20% to 76%.
Effective capacity planning in healthcare brings another fringe benefit. It frees practices staff from the tedious task of scheduling and coordinating appointments, allowing them—and their providers—to focus 100% of their efforts on direct patient care.
Gain additional capacity for your health system today
Your health system’s patients shouldn’t have to wait 31 days or longer to see the provider of their choice. With a capacity optimization strategy, you can convert more searches into appointments, attract new patients, and right-size your entire care portfolio.
Want to know where to begin? Explore this five-point framework for smarter capacity management. And if you want to talk with our team at DexCare to find the revenue opportunities within your capacity data, schedule a call with us today.
 Veterans Affairs
Veterans Affairs