Innovations in Streamlining Virtual Care Services
Derek Streat shares insight on how DexCare technology’s Get Care Now program in partnership with UR Medicine is finding ways to virtually connect patients with providers faster.
The podcast, PopHealth Perspectives, is produced by Integrated Healthcare Executive.
Read the full transcript:
Welcome back to PopHealth Perspectives, a conversation with the Population Health Learning Network where we combine expert commentary and exclusive insight into key issues in population health management and more.
In this episode, Derek Streat, Co-Founder, CEO, and Chairman of DexCare, joins us today to learn about how DexCare technology’s Get Care Now program in partnership with UR Medicine is finding ways to virtually connect patients with providers faster.
My name’s Derek Streat, I’m co-founder and CEO of DexCare. I’m a technology entrepreneur. I’ve been building companies for a couple of decades now, mostly in the healthcare IT space. I’ve also done some things in the AdTech, MarTech space and the social networking space as well. And DexCare is a company that we spun out of Providence Health System a couple of years ago after the project had been going for a few years inside of Providence and producing some really, really strong results inside of that organization so we spun it out and now we’re an independent organization.
What went into UR Medicine’s decision to choose new technology to help power the Get Care Now program?
Rochester, like a number of health systems around the country, are increasingly trying to find ways to cater to the convenience and accessibility of care for the patients in their regions. And at DexCare, we’re focused on ensuring that everyone everywhere has exceptional access to the best expertise to prevent, treat and cure illness. And one of the ways you do that is you make sure that healthcare access is really accessible and you can get it as quickly as possible, maybe even now if you need it. And so this is part of a broader strategy that UR Medicine has to not only make care available immediately in a virtual setting, but also across other modalities and settings as well, in a way that again speaks to the needs of consumers.
One of the other challenges with healthcare access these days, not only in Rochester but all over, is that once consumers and patients find that care, whether it’s online or calling a number or something like that, it’s not always optimized for the health system as well. And the providers as well. You can have everybody get access to care, but if the providers are already at capacity and burnt out or close to getting burnt out, that’s not going to work for the providers or the health system as well. So balancing that demand with that capacity, we call it orchestrating demand and supply, within health systems is really important as well to making healthcare access work. And as we increase the modalities in the settings that we partner with UR Medicine on to make health care accessible to everyone, that increases the opportunities to make sure that that matching is done in the right way that works for providers in the health system as well, which really the balancing of all the needs of those stakeholders is really what we believe is key to making healthcare access work in this country.
How has the implementation of these on-demand video visits improved the convenience of care for patients?
Well, for one, it allows you to get access to care for conditions where it’s appropriate in the comfort of your own home, on your mobile device, in your car, or wherever you are. But we don’t stop there. Part of it is having the capability to do that, and there are a number of virtual health telemedicine solutions out there. What we do to make it even more convenient and better for UR Medicine patients is make sure that once you’ve found that modality or way of getting care through Get Care Now that we can really minimize the friction for you as a patient to getting that care. And so that means ensuring that the minimal amount of data is picked up in the process, making sure we support guest flows if you don’t happen to have a MyChart account set up yet since they’re an epic shop. And then after the visit, coming back around and picking up those additional data, making sure that data is written into the EMR so that it works well for the health system as well.
All of those things that happened after you found this virtual care option are also important to make it more convenient for consumers. Streamline the process, minimal fields, minimal wait times, everything that we could do to get you in front of that provider as quickly as possible to take care of what you need, which is what’s most important. And we’ve found that all of that stuff makes a difference. So at UR Medicine, we’ve been able to find that these virtual visits are able to be done by those providers in about nine minutes. Because again, we can make sure that some of the work is offloaded to the technology and shared with the patient and provider in terms of filling out fields and getting information, and so forth. That adds up to real time because the national average for a virtual visit is about 13.8 minutes, and so you can literally get care faster if you are a UR Medicine patient going through a DexCare powered experience than you can if you’re working with a health system that does not have a DexCare powered experience. And that makes it fundamentally more convenient for patients.
Absolutely. I’m sure that really adds up and makes a difference. So what effect does this new technology have on the health system resources?
We had to take a very broad view of access. And the platform that we’ve created, again, this orchestration platform to orchestrate demand and supply and healthcare, really there are three legs of the stool, if you will, to making that platform work, making that orchestration work. One we’ve talked a lot about today, we call it digital discovery. And this is about making sure that your patients and even people before their patients or their consumers and beginning to start to consume care, making sure that they know you exist, they know your options exist, and it’s easy for them to get into care in those kind of streamlined flows I mentioned earlier.
The two other parts though of the system, we call intelligent navigation and capacity optimization, and those are all about ensuring that patients are routed to the safest best care option for them and that the resources within the health system are automatically allocated when and where they can be most productively employed. And that’s critical because as I was mentioning earlier, it’s important that patients have great experiences. And UR Medicine patients that are going through DexCare powered experience provide an average net promoter score of 92 out of a hundred. So we’re checking that box, very, very high satisfaction. But it’s got to work for providers in the health system as well. If providers are burnout or near burnout, they’re not going to be able to take care of those patients to the best of their ability and it’s not fair to them as well. And if health systems are not able to ensure that patients are routed to what’s called top of license, for example. If a nurse can take care of me just as well as a doctor and that nurse is available and she happens to be half as expensive to the health system as the doctor, then the nurse is who should see me.
And that’s important because that allows then the health system to use its resources more efficiently throughout the rest of the health system and for other patients and actually see more patients in the end. It’s important that if I’m matched up, that as a patient that the provider I see, or the service line I work with or the actual clinic I go to or the modality, virtual versus in person I use, it’s important that those are tuned to what is going to work best for me, the provider in the health system. So that, for example, I’m seeing providers that happen to see a lot of people like me, maybe the people that come in with a certain reason for visit, a certain consolation of conditions. We want to make sure that when I’m seeing that provider, I’m seeing a provider who’s seeing a lot of the same thing so that they can treat me as efficiently and effectively as possible. And so we do that routing. Behind the scenes, we’ve got a big decisioning engine that takes in these data from these different sources, trains up models to figure out what’s the best match between this patient and this provider setting service line modality or the intersection of those things. And the net result is health systems are able to see about 20 to 30% more net new patients into their system, and they’re able to increase their extended capacity of their existing resources by about 40% as a result of these technologies, which at the end of the day makes care more accessible because more patients can be seen now in a way that works for everybody, not just the patients, but the providers in the health system as well.
That’s very impressive, honestly, and in the way that it kind of benefits everyone in the system. And you’ve really touched on a few of these, but could you just summarize how these digital experiences are attracting new patients and reducing costs?
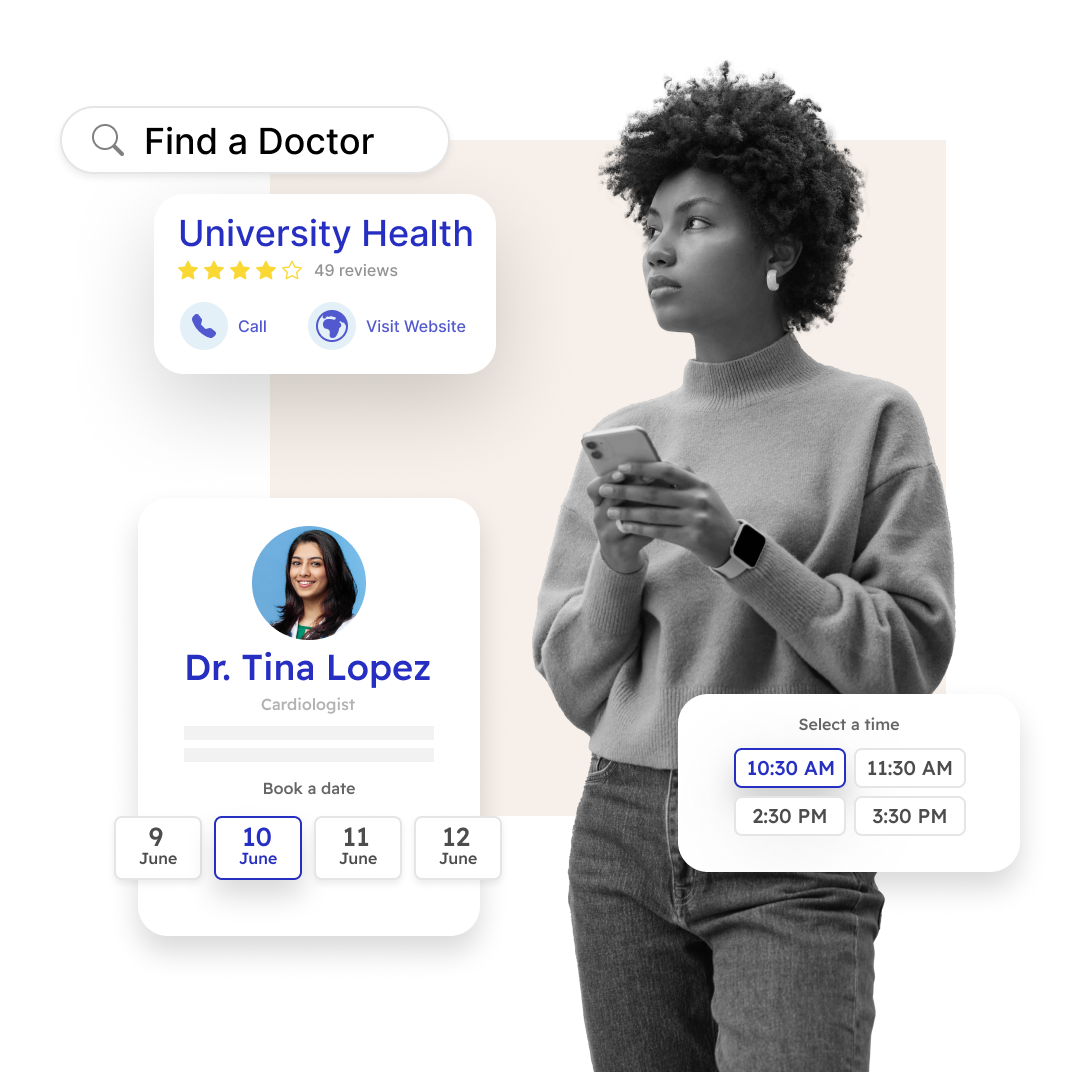
So on the digital discovery portion of our service, what that system is doing is it’s making sure that the availability of all the resources within the health system, providers, clinics, et cetera, are showing up in the places that consumers are looking for care. Contrary to what many, many health systems sometimes think, that’s typically not their website or their app. Some people go to their website or app, but most people live their digital lives on Google where they searched for things on various websites out there or various media sites. And so it’s important that the care, we call them care options that the health system has in this case with UR Medicine, we’re starting with virtual care. It’s important that those are distributed and made seeable to consumers and patients as they’re searching for care on Google and visiting other websites.
And then you go to find a doctor and you do a search and you see page after page of, in some cases, hundreds, thousands of doctors to treat a low acuity condition, for example. Instead of seeing that, what you’ll see in a DexCare powered experience is we probably can’t get it down to one option. You can’t have enough data to do that, but we can get it to a much more reduced set of options that are relevant to you. So you just have less noise and fewer things to have to kind of mine through to make a choice. And then we can provide alternatives. So in a DexCare powered experience, instead of seeing a bunch of doctors and finding a doctor, some of which you know may find out once you click on them that they’re actually not available, and then you got to go back out and search again. In our case you would find, here’s some doctors, maybe here’s the doctor, maybe here’s a doctor you were looking for, or maybe if you’re in the system, here’s your primary care doctor. But if that doctor’s not available, we can show you alternatives maybe in that clinic or other others that could see you faster or maybe more aligned with your particular situation you’re dealing with right then. And all of this is in service of making sure you get what you need as a patient as quickly and easily and easily as possible while doing all the other stuff I mentioned earlier, to make sure that the health system can actually service you in a productive and sustainable way for them.
That decision fatigue and having an overwhelming wealth of options there definitely is an issue. So for other health systems, do you see this as a platform that would be transferrable and also have benefits for them?
Absolutely. When we built this originally in Providence, the aim was to address specific challenges within the health system. Specifically, we had the picture that I was painting earlier of, it’s a very confusing environment of access points for patients. Lots of different options, the words all sounded kind of the same, you didn’t really know where to go, and the experiences were varied. And so we put that into single threaded experiences for all the kinds of care that we call provider agnostic care initially, care that is the majority of care that people get where you have pain, you have something and you just want it to get dealt with. You’re not really focused on a particular person, you just want this issue addressed. And in doing that, we were able to produce the kind of results that I mentioned earlier with new patients and capacity, et cetera.
The idea was always once it worked within Providence, then as a large Catholic nonprofit system, which the mission, Providence takes the mission very, very seriously. And part of the mission is to help improve the lives of everyone everywhere. And so it’s very both strategic and also just the right thing to do for us to be making this system available to health systems all around the country. And so that’s why we spun it out as a separate entity. And now we’re proud to say we power the experience, the consumer and backend experiences for organizations as large as Kaiser across all 50 states to the academic centers like the University of Rochester, obviously, and others to leading health system brands, regional brands like ACHN or THR, SSM, these kinds of health systems that are serving wide swaths of the population. I think last time we looked among our partners, right now, about 25% of the US population are within the catchment area of those health systems. Now, they don’t all go through DexCare experiences, but the point is those are patients in the market served by those health systems. And so it’s doing what it was intended to do, which is ensuring that everyone everywhere enjoys exceptional access to the best expertise to prevent, treat and cure illness. And it was always necessary to make sure that we were doing that with multiple health systems around the country. Because as big as Providence is, Providence doesn’t serve everybody everywhere. And so we’re doing what we set out to do.
Listen to More?
Unlock the latest healthcare insights through captivating podcasts featuring DexCare.
 Veterans Affairs
Veterans Affairs