Breaking the Capacity Bottleneck: How Care Orchestration Relieves the Pressure
Some providers are booked solid, others underutilized, while patients are stuck waiting. Capacity optimization is about fixing the supply and demand imbalance.
By aligning provider workload, care settings, and patient demand, organizations unlock hidden appointments, reduce bottlenecks, and drive significant revenue growth.

Breaking the Capacity Bottleneck: How Care Orchestration Relieves the Pressure
Some providers are booked solid, others underutilized, while patients are stuck waiting. Capacity optimization is about fixing the supply and demand imbalance.

Forces Shaping Health System Capacity
Competitive, economic, social, technological, and regulatory forces are putting new pressures on healthcare capacity. Health systems that adapt to these challenges can unlock efficiency, improve access, and drive sustainable growth.

Staffing Forces:
By 2052, nearly 84 million Americans will be over 65—almost double the number from a decade ago. At the same time, the ratio of healthcare workers to seniors is shrinking, dropping from 4:1 in 2010 to just 2.9:1 by 2030. Seeing a growing senior population with fewer providers to meet demand, can lead to an increased strain on health systems.
The Opportunity:
Invest in care orchestration, AI-driven efficiency, and digital tools to maximize workforce capacity and ensure patients get the right care at the right time.

Competitive Forces:
Private equity groups are buying up independent practices and specialty groups, siphoning business from profitable health system service lines. Meanwhile, the rise of “payvider” models is steering patients toward specific insurance networks and away from health systems. To compete, health systems must make care more accessible, convenient and efficient.
The Opportunity:
Systems that master capacity management will differentiate themselves with streamlined scheduling, more care options and optimized virtual care, helping retain current patients and attract new ones.

Economic Forces:
Operating margins are tight. Reimbursements are shrinking. Labor costs are rising. The only way for a health system to survive is to use its limited resources cost-effectively and efficiently.
The Opportunity:
By addressing capacity inefficiencies, health systems can lower overtime costs, tackle Emergency Department (ED) overuse, and reduce ED diversions.

Social Forces:
Younger patients expect seamless online scheduling, and quick access to care – when and where they need it. Older patients require more help managing chronic diseases, consuming more time and clinical support. And health systems are stuck in the middle balancing resources across low and high acuity care.
The Opportunity:
Effective capacity management breaks the logjam. Systems can see where provider schedules are overextended or underused, adjust them to free up more patient slots, and serve up those open slots online to increase access.

Technological Forces:
Innovations like AI, telehealth, and big data give health systems more tools than ever before to balance capacity, while eliminating data blind spots. But organizations that can’t adopt these tools quickly will fall behind fast, as evidenced by the fact that 90% of healthcare workers say they already use AI in some way.
The Opportunity:
With a single source of capacity data, health systems can implement AI and machine learning to automate capacity management, while also keeping a human in the loop at all times.

Regulatory Forces:
New and evolving regulations, including the No Surprises Act, create an urgent pivot point, whereby capacity isn’t just a challenge, but a federal mandate.
The Opportunity:
A flexible and holistic capacity management strategy allows health systems to manage in-network provider availability and improve scheduling, preventing costly out-of-network scenarios for patients.
Network-wide imbalances are causing delays in care and cutting into revenue.
Patients
Patients wait 26 days on average to access a primary care doctor
Providers
Some providers have more availability while others are overwhelmed
Modalities
Virtual care queues sit empty as urgent care waiting rooms bulge at the seams
Locations
One location struggles with massive scheduling backlogs, while another has empty slots
Network-wide imbalances are causing delays in care and cutting into revenue.
Patients
Patients wait 26 days on average to access a primary care doctor
Providers
Some providers have more availability while others are overwhelmed
Modalities
Virtual care queues sit empty as urgent care waiting rooms bulge at the seams
Locations
One location struggles with massive scheduling backlogs, while another has empty slots
5-Point Framework for Smarter Capacity Management
Based on best practices of leading health systems, this framework can help your organization pinpoint provider imbalances, find patient access gaps, and effectively balance provider supply with patient demand.
Step 1
Define your data needs, identify bottlenecks and find pockets of availability
Begin by assessing which capacity data you already track, and which types you need to track. As you conduct this assessment, ask:
What are our key data needs?
Can we accurately analyze patient demand, provider availability, scheduling patterns, and utilization rates? This means connecting multiple data sources, often governed by multiple people and disparate processes. Sources could include: EHR, practice management system, patient portal, insurance eligibility/verification system, provider directory/credentialing system, telehealth platform, and patient engagement/reminder systems.
What’s blocking our view of capacity?
Seek to identify any fragmented data sources, integration challenges, and other items that inhibit visibility across care settings. Health system data is often a mess of outdated and disorganized sources. Knowing the basics can be challenging: who works for your system, their specialties, addresses and phone numbers.
Which technologies will help us the most?
Assess your technology gaps and start investigating advanced analytics, predictive modeling, AI-powered dashboards and other tools that can help you surface actionable insights.


Step 2
Improve care access by routing to care venues with available resources
A full view of capacity data enables smart resource allocation, ensuring timely, efficient care while achieving health system goals.
For example, patients with low acuity concerns can be routed to same day care options.
Reduce overcrowding in the ED and urgent care
by using AI and data intelligence to assess patient needs and guide patients to the most appropriate care option.
Enable providers to practice at the top of their licenses
by routing appropriate cases to specialists and assigning routine visits to advanced practice clinicians.
Decrease provider burnout
by allowing providers to right-size their schedule and incorporate a mix of acuity levels into their workflows.
Step 3
Use real-time data to scale resources in alignment with predictable, seasonal trends
Predict anticipated spikes in patient demand—and respond appropriately—using data as your guide.
Analyze historical trends
to ramp up for flu season, school-year exams, or insurance coverage cycles.
Allocate staff resources proactively
by adjusting staffing levels in advance to meet peak demand.
Forecast the future
Incorporate forecasting tools to simulate scenarios and ensure your organization can meet unexpected surges.


Step 4
Pursue workforce optimization
Right-size provider schedules, ease staffing crunches, and reduce staff burnout by achieving better balance.
Visualize the provider spectrum
overburdened, optimized, and underutilized—and their implications on care delivery.
Assess the market impact of burnout
by comparing the cost of hiring new providers versus the cost of the tools you’ll need to optimize your current providers. Replacing a physician in a healthcare system can cost between $250,000 and $1 million or more.
Add up the bottom-line impact
Calculate how much you can save by redistributing just 5% of underutilized providers to address care gaps, improve access, and reduce unnecessary costs.
Step 5
Respond to changing behaviors and enhance the patient experience
Capacity maximization is the key to a better patient experience, allowing your health system to:
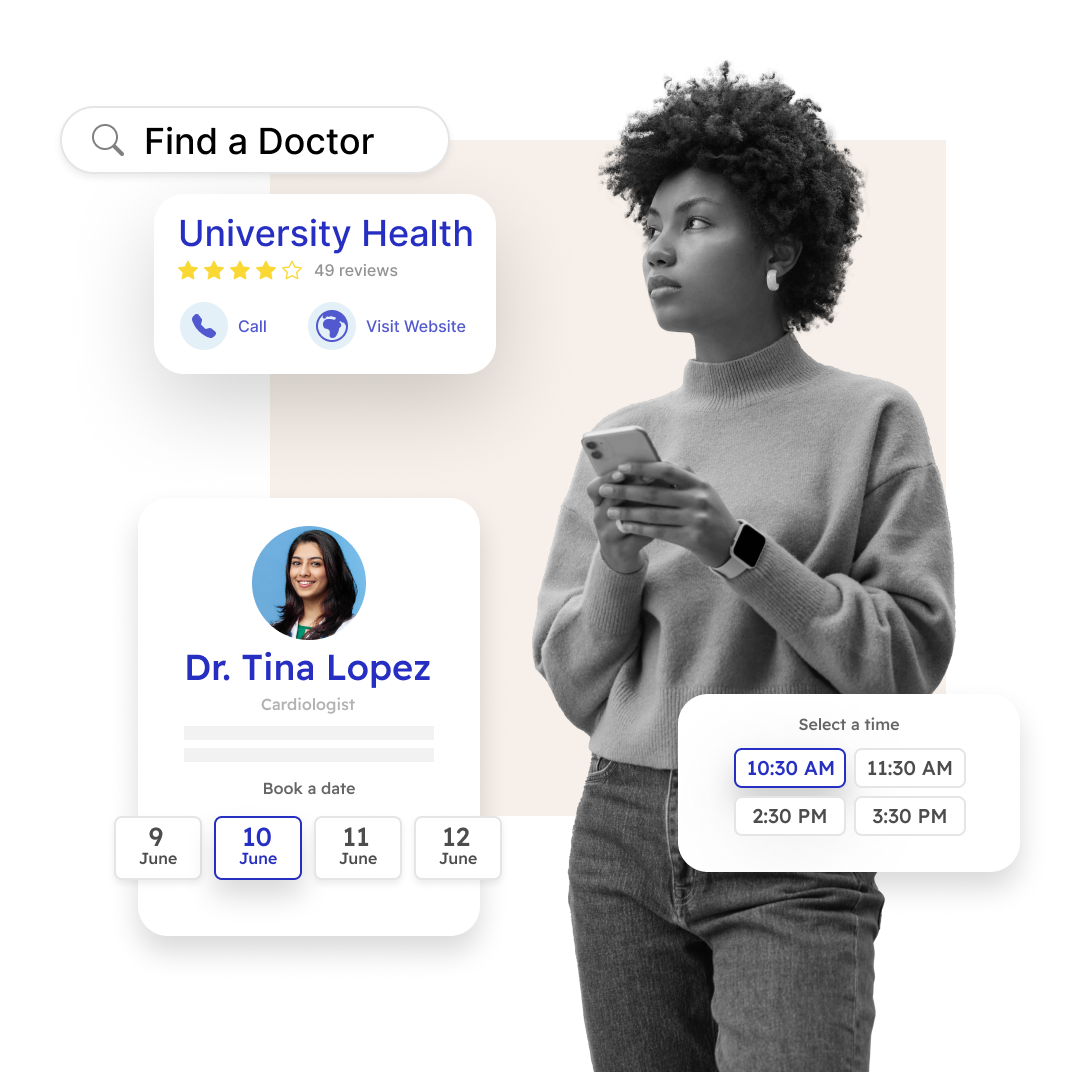
Retain current patients and attract net-new patients
by offering a more convenient and transparent booking experience that better meets their needs.
Surface real-time appointment availability
across providers, locations, and modalities, making care more convenient and boosting patient satisfaction and outcomes
Offer self-scheduling and best-fit care options
at every digital front door touchpoint, accelerating access, shortening wait times, and reducing no-show rates

5-Point Framework for Smarter Capacity Management
Based on best practices of leading health systems, this framework can help your organization pinpoint provider imbalances, find patient access gaps, and effectively balance provider supply with patient demand.
Step 1
Define your data needs, identify bottlenecks and find pockets of availability

Begin by assessing which capacity data you already track, and which types you need to track. As you conduct this assessment, ask:
What are our key data needs?
Can we accurately analyze patient demand, provider availability, scheduling patterns, and utilization rates? This means connecting multiple data sources, often governed by multiple people and disparate processes. Sources could include: EHR, practice management system, patient portal, insurance eligibility/verification system, provider directory / credentialing system, telehealth platform, and patient engagement / reminder systems.
What’s blocking our view of capacity?
Seek to identify any fragmented data sources, integration challenges, and other items that inhibit visibility across care settings. Health system data is often a mess of outdated and disorganized sources. Knowing the basics can be challenging: who works for your system, their specialties, addresses and phone numbers.
Which technologies will help us the most?
Assess your technology gaps and start investigating advanced analytics, predictive modeling, AI-powered dashboards and other tools that can help you surface actionable insights.
Step 2
Improve care access by routing to care venues with available resources

A full view of capacity data enables smart resource allocation, ensuring timely, efficient care while achieving health system goals.
For example, patients with low acuity concerns can be routed to same day care options.
Reduce overcrowding in the ED and urgent care
by using AI and data intelligence to assess patient needs and guide patients to the most appropriate care option.
Enable providers to practice at the top of their licenses
by routing appropriate cases to specialists and assigning routine visits to advanced practice clinicians.
Decrease provider burnout
by allowing providers to right-size their schedule and incorporate a mix of acuity levels into their workflows.
Step 3
Use real-time data to scale resources in alignment with predictable, seasonal trends

Predict anticipated spikes in patient demand—and respond appropriately—using data as your guide.
Analyze historical trends
to ramp up for flu season, school-year exams, or insurance coverage cycles.
Allocate staff resources proactively
by adjusting staffing levels in advance to meet peak demand.
Forecast the future
Incorporate forecasting tools to simulate scenarios and ensure your organization can meet unexpected surges.
Step 4
Pursue workforce optimization

Right-size provider schedules, ease staffing crunches, and reduce staff burnout by achieving better balance.
Visualize the provider spectrum
overburdened, optimized, and underutilized—and their implications on care delivery.
Assess the market impact of burnout
by comparing the cost of hiring new providers versus the cost of the tools you’ll need to optimize your current providers. Replacing a physician in a healthcare system can cost between $250,000 and $1 million or more.
Add up the bottom-line impact
Calculate how much you can save by redistributing just 5% of underutilized providers to address care gaps, improve access, and reduce unnecessary costs.
Step 5
Respond to changing behaviors and enhance the patient experience

Capacity maximization is the key to a better patient experience, allowing your health system to:
Retain current patients and attract net-new patients
by offering a more convenient and transparent booking experience that better meets their needs.
Surface real-time appointment availability
across providers, locations, and modalities, making care more convenient and boosting patient satisfaction and outcomes
Offer self-scheduling and best-fit care options
at every digital front door touchpoint, accelerating access, shortening wait times, and reducing no-show rates
Struggling with seeing your provider imbalances? We can help you break it down.
Our data-driven capacity analysis uncovers hidden inefficiencies and revenue opportunities within your system.
- Find untapped capacity
- Optimize provider schedules
- Unlock new revenue streams
Get your personalized capacity report and start balancing your network today.

Struggling with seeing your provider imbalances? We can help you break it down.

Our data-driven capacity analysis uncovers hidden inefficiencies and revenue opportunities within your system.
- Find untapped capacity
- Optimize provider schedules
- Unlock new revenue streams
Get your personalized capacity report and start balancing your network today.
 Veterans Affairs
Veterans Affairs